We spoke to my chemotherapy doctor today, and my outlook is still great. He went over the results of a recent blood test, and while he noted that I am still technically in the recovery period from my surgery, there are no new causes for alarm, and he seemed pleased that I’ve been able to get out and do the things this summer. Afterward, I said to Lori that I felt like I’d let out a breath I didn’t know I was holding. Not that I’ve been worrying a lot about my health, but I haven’t…not been worrying about it either. It was nice to have such a relaxed, positive appointment.
Next steps will be a CT scan shortly after Christmas, likely with another blood test to compare results, and a colonoscopy in February 2026. I have adjusted quite a lot to having a stoma, but the thought of a scope going in makes me incredibly uncomfortable. I suspect it will continue to do so until well after the scope is completed. I’m not worried about anything in particular, I just hate the thought. So let’s not think it for the rest of the year! Hooray!
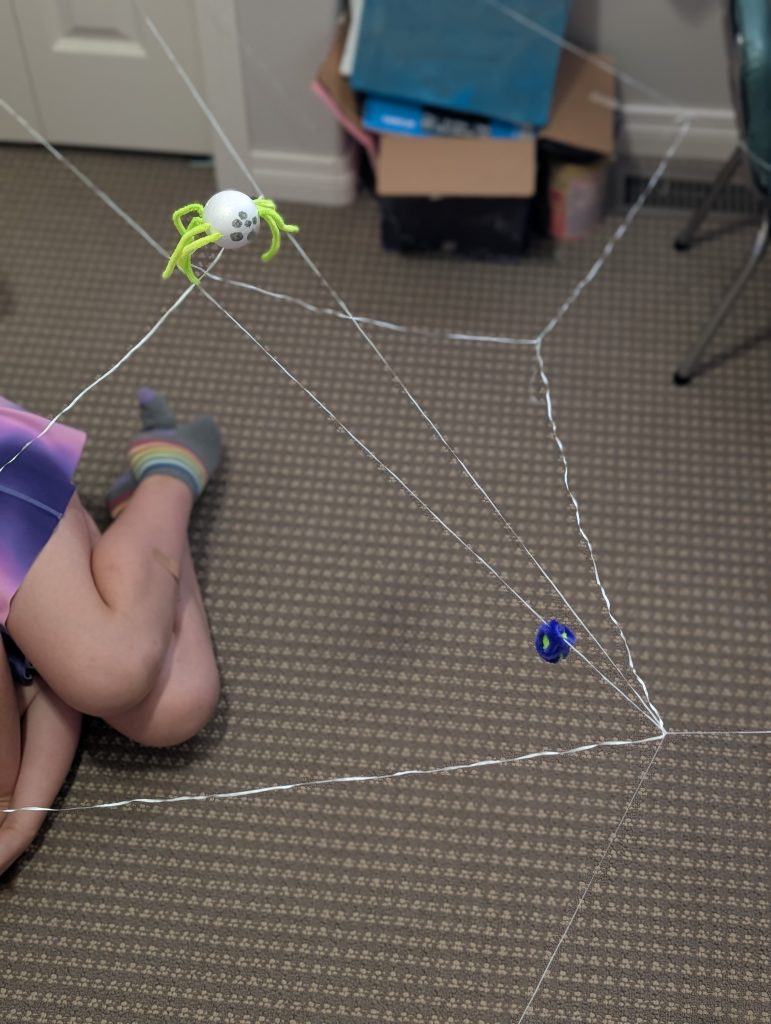
I’m still in counseling; the latest point of discussion is that I’ve been getting uncomfortable and sad when I look at younger photos of myself or others. In talking it through I’ve come to realize that I see these photos in a bittersweet way, now. There’s nostalgia, but it’s followed by a sadness when I think about the ways those people from the past are going to suffer and don’t know what’s coming. On my counselor’s advice I’ve been trying to turn that script around and remind myself how much of a blessing it is to have a happy past to look back on, and good things in your life to remember. It isn’t easy and I haven’t practiced it very much. I’m treating the exercise like a…what do you call that therapy for like, arachnophobes? Where you slowly spend more and more time with a spider? Exposure Therapy, I think. Except what I’m doing is not so systematic.
Overall, though, this summer has been grand. Not every day has been perfect, and I have not responded perfectly to every setback. But the good days have vastly outnumbered the challenging ones, and the thing I keep thinking, and saying aloud, is that whatever this summer turns out to be, it’s better than the one I survived in 2024. Maybe I can hold that thought for the rest of my summers, too.
Did you know? You too, dear reader, have also survived all of your worst days! You did it! Now keep going!
We went as a family to the Assiniboine Park Zoo on the August long weekend, and of course this meant a trip through the Polar Bear area. The polar bears have a large grassy area to wander around on, and then a rock-lined pool to dip into and swim around. There’s a clear tunnel for humans beneath the pool, and if you’re lucky, you can get up close to the bear as it splashes and swims about.
When we neared the tunnel, only the bear’s butt was underwater. I chuckled, wondering if that was all we’d get. The tunnel is crowded, so you naturally have to slow down a bit to get through and keep all of your loved ones nearby. I was last in line, and as I moved through, the bear suddenly dropped entirely into the pool, pushed off of the rocky wall, and glided directly over my head.
What a mixture of delight, awe, and gratitude I felt! I was almost moved to tears by the experience. I could only stand and watch as it swam away. Getting to observe this bear up close is just one of the many things left to see and do in this world, and I felt so blessed to be able to do this and (hopefully) much more.

And so, we come to the last part of this post, which is an announcement: I’ve decided that this blog has run its course, and this is likely to be the final post. I’ve felt for a couple of weeks that this time was drawing near, but I wanted to wait for the followup conversation with my doctor to seal the deal. This was started as a way to process my experiences and keep people in the loop, and, well, there’s not much of a loop in which to keep people anymore. This is a good thing, actually! I’m still growing and learning and adjusting, but I think I’m on to a new chapter now. If you want to know how that’s going, you’ll have to read my regular blog (which will be updated much less frequently than this one). Or, y’know, ask me in person!
As I wind this down, I want to say thanks one more time to June for the nudge to start blogging my journey. Like I said, it has been a great creative outlet and good for my mental health as well. Thanks one more time to everyone who commented here, on my various social medias, or in-person. Even if it was just to nudge me while I was at the shops, and say “I’m following your blog and praying for you,” your support was so very appreciated. Thanks to Cassidy in particular for every time I was allowed to use her photo in a post; she’s normally very averse to sharing her pictures online, and rightfully so! And last but certainly not least, thanks to my darling wife Lori, who proofread (nearly) every post to keep me factually accurate and point out when I stopped making sense. Any remaining errors are her fault, actually.
One of the last things I wrote about on my regular blog, a mere two days before getting my cancer diagnosis, was the phrase: “Being alive is as special an occasion as it gets.” It was true then and true now, and I hope that if you’re reading this, you agree too. Praise the Lord for every new morning we get to experience on this weird old Earth!
Thanks for reading! Goodbye for now!